A 55 year old male with SOB
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
A 55 year old male, farmer by occupation and a resident of rajammagudam, came with the chief complaints of
* Shortness of breath since 1 week
* Pedal edema since 3 days
* Decreased urine output since 3 days.
HISTORY OF PRESENTING ILLNESS
* The patient was apparently assymptomatic 3 years back when he was diagnosed with diabetes when he visited the hospital with complains of fever. He was given tablet pioplus-2(Glimepiride, Metformin and Pioglitazone). He is compliant with his medication.
1 year ago patient was having blurring of vision and dizziness for which he went to the doctor and was diagnosed with hypertension and was given amlodipine. He is compliant with the medication.
The patient complains of shortness of breath since 1 year. It was initially of grade 2(MMRC Classification) that is he has to stop to take breath while walking at his own pace. For this he went to a local doctor and was given a tablet (unknown).
- The shortness of breath has aggrevated to grade 4 MMRC classification
- The shortness of breath was associated with PND and orthopnea. It was not associated with chest pain or palpitations.
- The patient also complains of non productive cough since 3 days.
The patient has had decreased urine output for the past three days. In the 24hrs before admission he did not have any urine output.
- He doesn’t have any hesitancy, increased frequency or fullness of bladder.
Pedal edema since 3 days
He had first session of dialysis on the day of admission 19/02/22 ( indication was metabolic acidosis ph 7.19)
Other two sessions on 20/02/22 and 21/02/22
PAST HISTORY
he was diagnosed with diabetes 3 years ago when he visited the hospital with complains of fever. He was given tablet pioplus-2(Glimepiride, Metformin and Pioglitazone). He is compliant with his medication.
diagnosed with hypertension 1 year ago and was given amlodipine. He is compliant with the medication.
He is not a known case of coronary artery diseases, Asthma, TB, epilepsy.
PERSONAL HISTORY
Appetite: decreased
Diet : mixed
Bowel: normal
Bladder : decreased urine output
Sleep: disturbed
Addictions: nil
GENERAL EXAMINATION :
Patient is conscious,coherent,cooperative coherent, cooperative and well oriented to time and place
Moderately built and nourished
Pallor is present
No signs of Icterus, cyanosis, clubbing, edema, lymphadenopathy
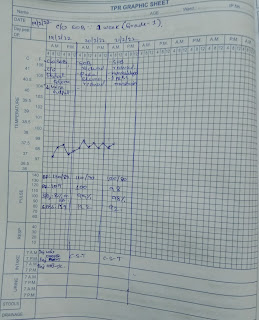
Vitals : PR - 62bpm
RR - 20cpm
BP - 110/80mmHg
Afebrile
RESPIRATORY SYSTEM :
Inspection :
Chest is bilaterally symmetrical
Bilateral air entry present ,equal expansion on both sides
Position of trachea is central
Supraclavicular and infraclavicular hollowness is not seen
Crowding of ribs is not seen
No visible scars, sinuses, pulsations
Palpation :
Expansion of chest is equal on both sides
Trachea is central
Vocal fremitus: resonant note felt
Percussion:
All the lung areas were resonant
Auscultation :
Normal vesicular breath sounds heard on both sides
Vocal resonance :resonant in all areas
CARDIOVASCULAR SYSTEM :
JVP:
appears raised
INSPECTION :
shape of the chest is elliptical ,symmetrical
No precordial bulge, scars, sinuses,dialated veins
No visible pulsations
PALPATION :
Apex beat felt in 6th intercoastal space
No parasternal heave
AUSCULTATION :
S1, S2 heard, no murmurs
PER ABDOMEN :
soft, nontender
No helatosplenomegaly
CNS: imtact

















Comments
Post a Comment